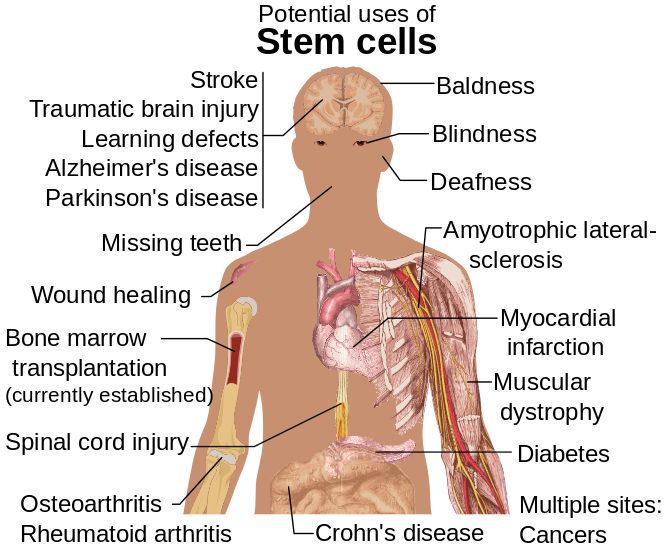
A recent Google alert served up links to articles on several new developments in progress in the world of stem cell research. In addition to discussion of funding for using stem cells to grow “clean meat,” recent work Happily, there seems to be no end to the number of areas in which humankind will at least seek solutions, if not actually develop workable applications, using this magical tool straight from nature.
Healing with stem cells (Abilene Recorder Chronicle). …”stem cell therapy ‘pennies on the dollar’ when it comes to treatment. ‘Healing is the returning the individual into function and Trinity’s research is focused … ‘Stem cells are light switches to the inflammatory process.
How men continually produce sperm — and how that discovery could help treat infertility (Science Daily). “This advance, the researchers write, opens the possibility that spermatogonial stem cell transplants could be developed to treat male infertility,..”
Kidneys grown in rats could pave way for human transplant options (The Japan Times). The research, published Wednesday in the Nature Communications journal, … The researchers found that the mice stem cells produced apparently